A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Air Leaks in the Newborn
The lungs inflate, or fill with air, as you breathe. In the lungs, air travels through branching airways called bronchial tubes. These end in tiny sacs called alveoli. Sometimes alveoli rupture. This causes air to leak into the space between the lungs and the chest wall. These air leaks cause problems with breathing and can lead to lung damage.
What causes air leaks?
Any baby can get an air leak. Air leaks may occur due to:
-
Being on a ventilator (breathing machine) for a breathing problem. The pressure of the air from the ventilator can cause alveoli to rupture.
-
Meconium aspiration syndrome. This is when an infant inhales a bit of meconium, or its first feces, during or after labor. It causes the lungs to become irritated, damaged, and overinflated (filled with too much air).
-
Respiratory distress syndrome. This common problem in premature babies is from immature lung development. It causes trouble breathing.
-
Vigorous crying, which causes the alveoli to rupture. Some babies cry hard enough to do this at birth, or soon after.
-
Lung problems that need the baby to work harder to breathe
-
Congenital problems, such as an underdeveloped lung
-
Unknown causes
The main types of air leaks
Pulmonary interstitial emphysema is when tiny ruptures occur in the alveoli. This problem allows air to leak out into the lung tissue. That puts pressure on the surrounding alveoli. Too many of these tiny leaks can lead to these more severe problems:
-
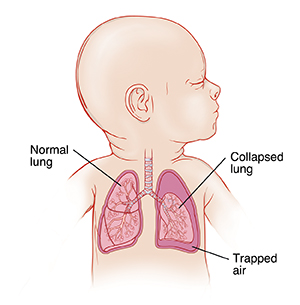
Pneumothorax (collapsed lung). Air gets trapped between the chest wall and the lung. This trapped air puts pressure on the lung, preventing it from inflating. The baby then has trouble breathing.
-
Pneumomediastinum. Air leaks into the chest, into the space between the 2 lungs and around the heart.
How are air leaks treated?
Your baby’s treatment will depend on how severe the air leak is. If the baby is not having breathing problems, treatment probably isn’t needed. A small air leak may heal by itself. For more severe cases, your baby may need one of these treatments:
-
A needle or catheter (small, flexible tube) is put into the space between the lungs and the chest wall. It is used to draw air out. This process helps remove the air that leaked out, so breathing can return to normal. If a lot of air leaked out, though, more treatment may be needed.
-
A chest tube is put into the space between the lungs and the chest wall. The chest tube is attached to a suction device that pulls out the trapped air, so the lungs can expand once again. This treatment lets the tear heal. It may take a few days for the tear to heal. The chest tube will stay in during this time.
-
The baby may need breathing support (such as supplemental oxygen or a ventilator) until the air leak heals.
What are the long-term effects?
In most cases, once an air leak is treated, there are no lasting problems. If a chest tube must be used, rare complications, such as internal bleeding or puncture of the lung could occur. Some babies with air leaks go on to have long-term breathing problems. The healthcare provider can give you more information about your baby.
Online Medical Reviewer:
Donna Freeborn PhD CNM FNP
Online Medical Reviewer:
Heather M Trevino BSN RNC
Online Medical Reviewer:
Liora C Adler MD
Date Last Reviewed:
10/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.